Why Diabetic Eye Disease is Often Silent
You might wonder why eye problem in diabetic patients do not always cause noticeable symptoms at first. This is because the retina has a lot of nerve cells but fewer pain receptors. So, even if there is damage happening in your eyes, your brain may not register it as pain or discomfort. Over time, as the condition progresses, you might experience blurry vision or see dark spots, but by that time, the disease may already be more advanced. This is why it's vital to schedule regular eye exams, even if you feel fine.
Even worse for some patients, blurring of vision can happen out of sudden. It is very important to understand that one doesn’t have to go blind just because they have diabetes.
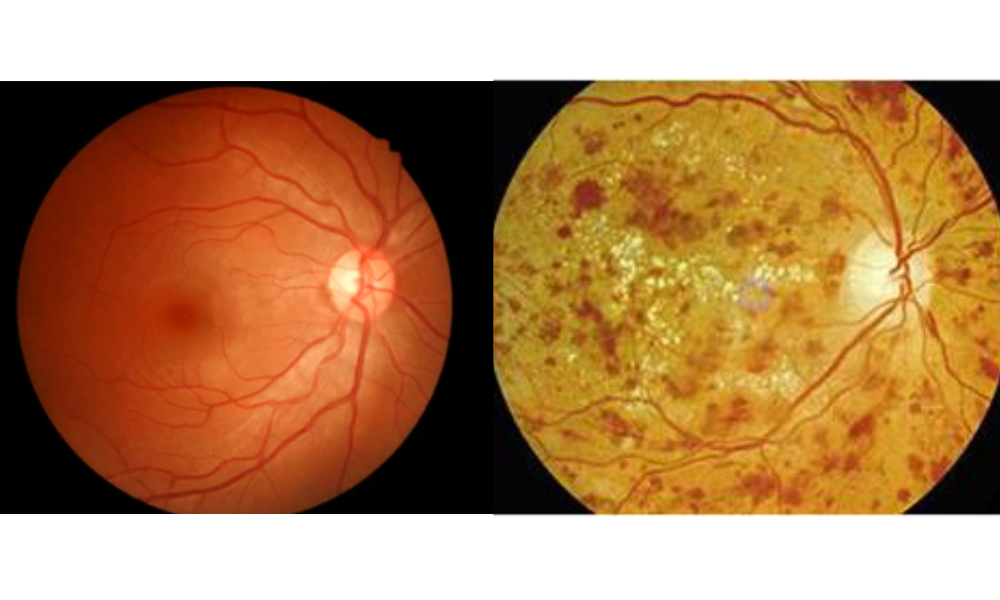
What Is Diabetic Retinopathy?
In simple terms, diabetic retinopathy is a condition that affects the blood vessels in the retina, the light-sensitive layer at the back of your eye. The retina helps send images to your brain, so it’s a crucial part of your vision. When someone has diabetes, high blood sugar levels can damage the blood vessels in the retina over time, leading to vision problems. It’s one of the leading causes of blindness in adults, but don’t panic – it’s preventable with the right steps.
How Does Diabetes Affect Your Eyes?
When blood sugar is consistently high, it can harm the blood vessels throughout your body, including the tiny ones in the eyes. In the retina, this damage leads to several changes:
1. Leaky Blood Vessels: High blood sugar can cause the small blood vessels in the retina to weaken and leak fluid. This causes swelling and can affect your vision.
2. New Blood Vessel Growth: In some cases, the retina tries to repair itself by growing new blood vessels. However, these new vessels are often weak and fragile, which can lead to more bleeding, scarring, and further vision loss.
3. Retinal Detachment: In severe cases, the damaged blood vessels and scar tissue can cause the retina to detach from the back of the eye, leading to permanent vision loss.
But don’t worry, just because diabetes affects your eyes doesn’t mean you’re doomed to vision problems. By managing blood sugar levels and getting regular eye check-ups, you can help protect your vision.
Symptoms of Diabetic Retinopathy
In the early stages of diabetic retinopathy, you might not notice any symptoms, which is why regular eye exams are so important. However, as the condition progresses, you might experience:
Blurry or wavy vision
Seeing spots or floaters
Difficulty seeing at night
Sudden vision loss
Dark or empty areas in your vision
If you notice any of these symptoms, it’s essential to see an eye doctor right away. The earlier diabetic retinopathy is detected, the more effective treatment can be.
Risk Factors for Diabetic Retinopathy
Not everyone with diabetes will develop diabetic retinopathy, but certain factors can increase the risk. These include:
Duration of Diabetes: The longer you've had diabetes, the higher your risk of developing retinopathy. People with type 1 diabetes are especially at risk if they’ve had it since childhood.
Blood Sugar Control: Keeping blood sugar levels in check is the most important way to prevent or slow down the development of diabetic retinopathy. Poor blood sugar control increases the risk of damage to the blood vessels in the eyes.
High Blood Pressure: Having high blood pressure along with diabetes can significantly increase the risk of eye problems, including diabetic retinopathy.
High Cholesterol: High levels of cholesterol can contribute to the damage of blood vessels, including those in the eyes.
Pregnancy: Women who have diabetes during pregnancy are at an increased risk of developing diabetic retinopathy, especially if their blood sugar levels are poorly controlled.
Genetics: If you have a family history of diabetic eye disease, you may be more likely to develop retinopathy yourself.
How to Protect Your Eyes If You Have Diabetes
The good news is that with proper care, you can reduce the risk of diabetic retinopathy or prevent it from worsening. Here are some tips to keep your eyes healthy:
1. Keep Your Blood Sugar Under Control
Managing your blood sugar is the most important step you can take to prevent diabetic retinopathy. Work closely with your doctor to develop a plan for maintaining healthy blood sugar levels through diet, exercise, and medication.
2. Monitor Your Blood Pressure and Cholesterol
High blood pressure and high cholesterol can worsen diabetic retinopathy, so it’s important to keep these in check. Eat a heart-healthy diet, exercise regularly, and take any prescribed medications to manage these conditions.
3. Get Regular Eye Exams
The American Diabetes Association recommends that people with diabetes get a comprehensive eye exam at least once a year. Even if you’re not experiencing any symptoms, early detection of diabetic retinopathy can help prevent vision loss.
4. Quit Smoking
Smoking increases the risk of diabetic retinopathy and other diabetes-related complications. If you smoke, talk to your healthcare provider about ways to quit.
5.Eat a Healthy Diet
Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help keep your blood sugar levels stable. Some research suggests that certain nutrients, like omega-3 fatty acids and antioxidants, might help protect the retina.
6. Exercise Regularly
Exercise helps regulate blood sugar levels and improves circulation. Aim for at least 30 minutes of moderate exercise most days of the week. Always check with your doctor before starting any new exercise routine, especially if you have other health concerns.

Treatments for Diabetic Retinopathy
If you’re diagnosed with diabetic retinopathy, don’t lose hope – treatments are available. The specific treatment depends on the stage of retinopathy and the severity of the damage. Some common treatment options include:
1. Laser Treatment: This is used to shrink or seal leaking blood vessels in the retina. It’s most effective in the earlier stages of retinopathy.

2. Injections: Medications can be injected into the eye to reduce swelling and prevent further damage to the retina. These are often used in more advanced stages of the disease.
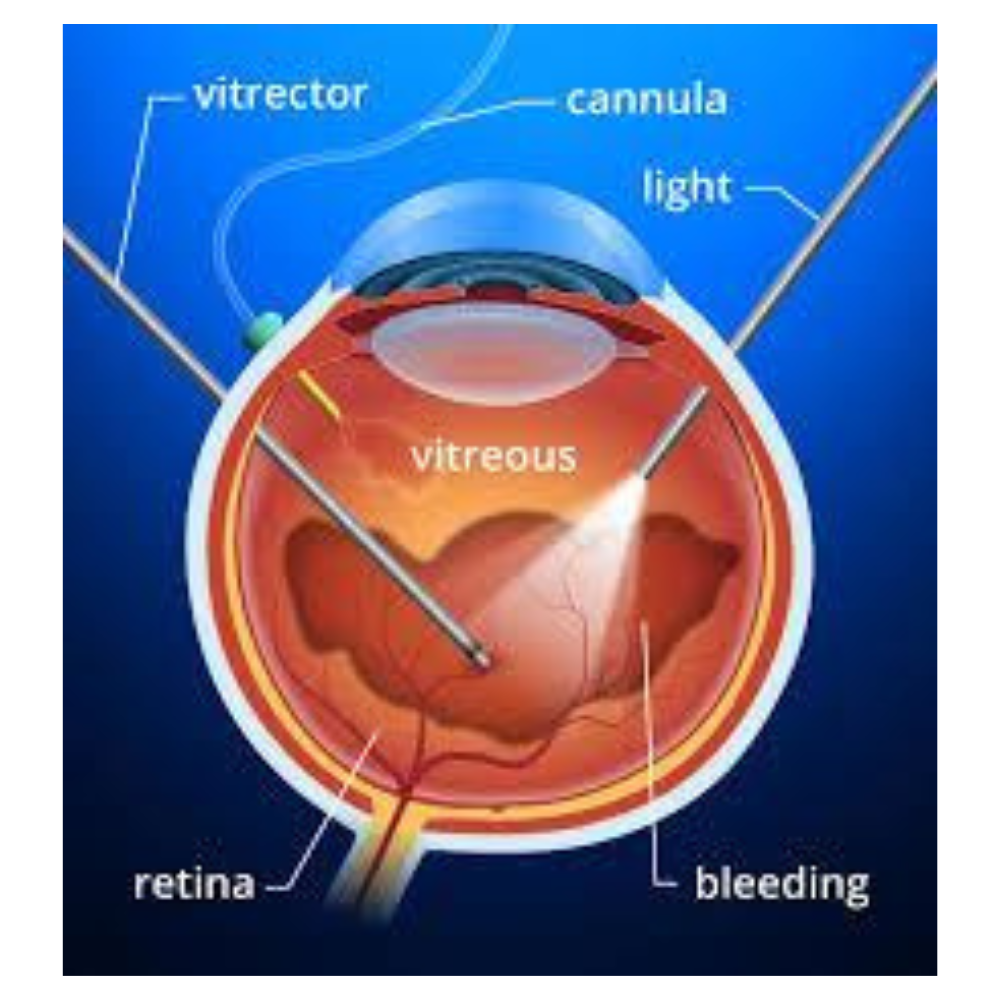
3. Surgery: In cases where bleeding has caused significant damage to the retina, a vitrectomy may be performed. This surgical procedure removes the blood-filled vitreous gel and replaces it with a clear fluid: https://www.kpjhealth.com.my/cfs/vitreoretinal
4. Monitoring: For some people with mild retinopathy, no immediate treatment is necessary, but regular monitoring is important to catch any changes.

Visit our centre for eye examination and treatment or browse through KPJ Centre For Sight website and social media pages: Facebook, Instagram and TikTok for more info.
Article by: Dr Mushawiahti Mustapha, Retinal Specialist MD UKM, Master of Surgery UKM, Fellowship in Vitreoretinal Diseases (Australia)

This content is provided by KPJ Centre For Sight.
The views expressed here are those of the author/contributor and do not necessarily represent the views of Malaysiakini.
Interested in having your press releases, exclusive interviews, or branded content articles on Malaysiakini? For more information, contact [email protected] or [email protected]

